What is Schizophrenia?
Definition and Overview
Schizophrenia is a chronic, severe mental illness characterized by distortions in thinking, perception, emotions, language, sense of self, and behavior. It falls under the category of psychotic disorders and typically emerges in late adolescence or early adulthood. Individuals with schizophrenia often experience hallucinations, delusions, disorganized speech, and impaired cognitive function.
How it Affects Brain Function and Perception
Schizophrenia disrupts normal brain chemistry and neural connectivity, primarily affecting the dopaminergic pathways. Functional imaging studies reveal abnormalities in the frontal cortex and limbic areas, correlating with emotional regulation and executive function impairments.
Myths and Misconceptions
- Myth: People with schizophrenia have split personalities.
Fact: Schizophrenia is not the same as Dissociative Identity Disorder. - Myth: Schizophrenia is caused by poor parenting.
Fact: While environment matters, it is not a sole cause. - Myth: All people with schizophrenia are dangerous.
Fact: Most individuals are non-violent and more at risk of self-harm.
Types of Schizophrenia
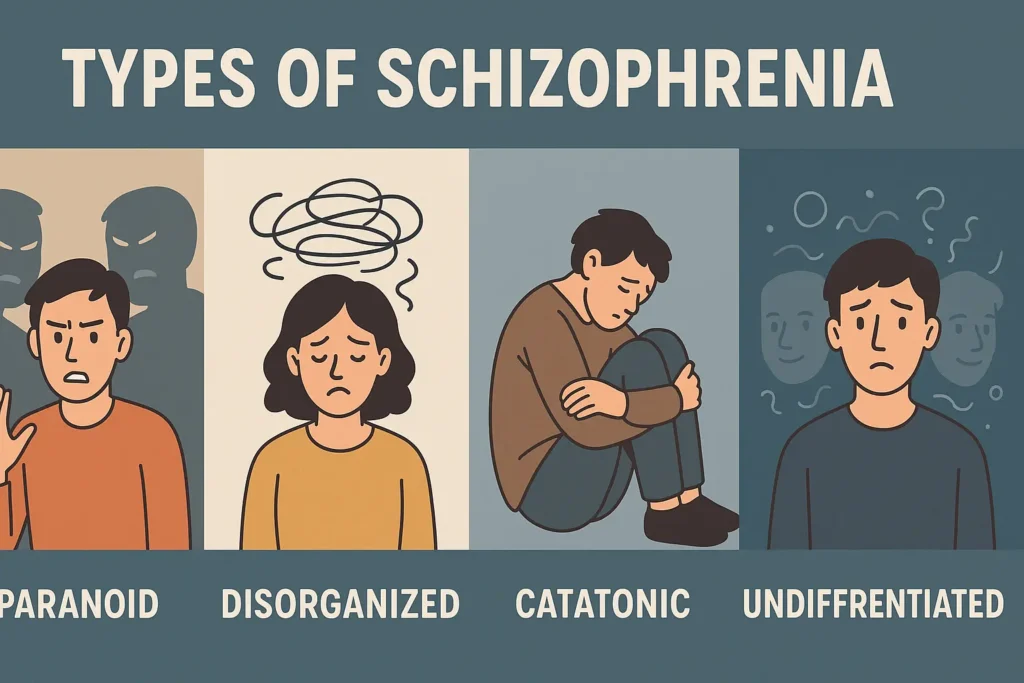
Paranoid Type
Dominated by delusions of persecution or grandeur and auditory hallucinations.
Disorganized Type
Marked by disorganized speech and behavior, flat or inappropriate affect.
Catatonic Type
Characterized by motor disturbances, ranging from immobility to excessive movement.
Undifferentiated Type
Meets general schizophrenia criteria but does not fit other specific types.
Residual Type
Individuals show signs of the illness without prominent positive symptoms.
DSM-5 Updates
The DSM-5 no longer classifies schizophrenia into subtypes. Instead, it uses a dimensional approach evaluating symptom severity across core domains.
Early Signs and Core Symptoms
Positive Symptoms
- Hallucinations (especially auditory)
- Delusions (persecutory, grandiose)
- Disorganized thinking and speech
Negative Symptoms
- Affective flattening
- Alogia (poverty of speech)
- Anhedonia and avolition
Cognitive Symptoms
- Poor executive function
- Difficulty with attention
- Impaired working memory
Behavioral Patterns with Real-Life Examples
- A student suddenly starts withdrawing socially, believes classmates are spying on him, and begins muttering to himself.
- A homemaker becomes paranoid that neighbors are trying to poison her food and locks herself indoors.
Causes and Risk Factors
Genetics
A strong hereditary component. First-degree relatives have a higher risk.
Neurochemical Imbalances
- Dopamine Hypothesis: Overactivity in mesolimbic pathways linked to positive symptoms.
- Glutamate Hypothesis: NMDA receptor dysfunction may contribute to cognitive deficits.
Environmental Influences and Trauma
- Prenatal exposure to viruses
- Complications during birth
- Childhood trauma
- Cannabis use in adolescence
Diagnosis and Clinical Evaluation
DSM-5 Criteria
Diagnosis requires two or more of the following for at least one month, with continuous disturbance for six months:
- Delusions
- Hallucinations
- Disorganized speech
- Disorganized or catatonic behavior
- Negative symptoms
Differential Diagnoses
- Bipolar disorder with psychotic features
- Major depressive disorder with psychosis
- Substance-induced psychotic disorder
- Schizoaffective disorder
Role of Neuroimaging and Psychometric Testing
- MRI and CT to rule out structural abnormalities
- Neuropsychological testing to assess cognitive deficits
- EEG to rule out seizure disorders
Conventional Treatment Options
Antipsychotic Medications
- Typical antipsychotics: Haloperidol, Chlorpromazine
- Atypical antipsychotics: Risperidone, Olanzapine, Clozapine
Cognitive Behavioral Therapy (CBT)
Helps patients challenge delusions and improve reality testing.
Psychosocial Support and Rehabilitation
- Occupational therapy
- Supported employment
- Peer support groups
Role of Hospitalization and Emergency Care
- For acute psychotic episodes
- Risk of harm to self or others
- Non-compliance with treatment
Homoeopathic Treatment for Schizophrenia

Philosophy of Homoeopathy in Mental Health
Homeopathy treats the individual as a whole, focusing on mental, emotional, and physical symptoms. Mental illness like schizophrenia is seen as a constitutional disturbance requiring personalized remedies.
Importance of Individualized Treatment
No two schizophrenic cases are alike. A thorough case history, including mental state, dreams, fears, and life history, guides remedy selection.
Commonly Used Remedies with Indications
- Anacardium Orientale: Dual personality, suspicion, auditory hallucinations
- Stramonium: Frightful hallucinations, fear of darkness, violence
- Hyoscyamus Niger: Loquacity, jealousy, indecent behavior, suspicion
- Lachesis: Delusional jealousy, talkativeness, religious mania
- Cannabis Indica: Time distortion, paranoia, extreme sensory perception
- Veratrum Album: Religious delusions, grandiosity, manic behavior
Clinical Considerations and Role in Long-Term Management
- Regular follow-up is essential
- Remedies may change based on symptom evolution
- Coordination with conventional care advised
Disclaimer: Homoeopathic medicines must only be prescribed by qualified professionals.
Holistic and Supportive Measures
Diet, Sleep, Lifestyle Factors
- Omega-3 fatty acids, B-vitamins
- Regular sleep-wake cycle
- Avoidance of stimulants and alcohol
Role of Mindfulness and Structured Routine
- Mindfulness meditation reduces anxiety
- Daily routine stabilizes mood and sleep
Family and Caregiver Support
- Psychoeducation
- Communication training
- Crisis management planning
Living with Schizophrenia
Daily Life Challenges
- Adherence to medication
- Stigma and social isolation
- Cognitive difficulties
Employment and Social Reintegration
- Supported employment models
- Role of NGOs and government programs
Stories of Recovery and Hope
Recovery is possible. With the right treatment, individuals can lead fulfilling lives. Many have returned to work, formed relationships, and even advocated for mental health awareness.
Frequently Asked Questions
- Can schizophrenia be cured?
Schizophrenia can be managed effectively, but it is typically a lifelong condition. - What is the difference between schizophrenia and bipolar disorder?
Schizophrenia involves psychosis consistently; bipolar disorder has mood swings with or without psychosis. - Is schizophrenia hereditary?
Genetics play a strong role but are not the sole factor. - Can homoeopathy help in schizophrenia long-term?
Yes, with individualized treatment and regular follow-up. - What age does schizophrenia usually appear?
Late teens to early 30s. - What are the early warning signs?
Social withdrawal, unusual beliefs, and cognitive decline. - Are antipsychotic drugs necessary?
Often, especially in acute phases. - Can a person with schizophrenia live independently?
Yes, with support and consistent treatment. - How is schizophrenia diagnosed?
Clinical evaluation based on DSM-5 criteria. - What are delusions and hallucinations?
False beliefs and sensory perceptions without external stimuli. - Can stress trigger schizophrenia?
Yes, especially in predisposed individuals. - What is psychosis?
A mental state involving loss of contact with reality. - Is hospitalization always necessary?
Only during severe episodes or safety concerns. - How does CBT help?
It helps in managing distorted thoughts and improving function. - Can diet influence schizophrenia?
Yes, certain nutrients support brain health and reduce symptoms.
Conclusion
Schizophrenia is a complex mental illness that affects thoughts, emotions, and behaviors. Early diagnosis, combined treatment modalities, and supportive care can dramatically improve outcomes. Homoeopathy offers an individualized and holistic approach, complementing conventional strategies.
Call to Action: If you or a loved one is showing signs of schizophrenia, consult a qualified mental health professional or a licensed homoeopathic physician. Early intervention makes a difference.